- 0086-571-85302990
- sales@greenskybio.com
Experts Urge Shift From Benadryl to Safer Allergy Drugs
2025-07-31
Benadryl has occupied medicine cabinets since the 1940s, but a growing number of allergists say the familiar pink tablets are overdue for retirement. In a viewpoint published in the World Allergy Organization Journal, physicians argue that diphenhydramine’s sedating and cardiac side-effects, coupled with abuse potential, make the first-generation antihistamine unsuitable for over-the-counter sale.1
“If it went before regulators today, I doubt it would clear the bar for OTC status,” said Lawrence Schwartz, MD, PhD, an allergy specialist at Virginia Commonwealth University who was not involved in the paper.
What Benadryl does—and why it differs
Diphenhydramine blocks histamine H1 receptors throughout the body, calming runny noses, watery eyes and hives. Unlike newer “second-generation” antihistamines—loratadine (Claritin), cetirizine (Zyrtec) and fexofenadine (Allegra)—it easily crosses the blood-brain barrier, causing pronounced drowsiness.4 It also interferes with acetylcholine, sodium and potassium channels, which can trigger dry mouth, constipation, urinary retention, blurry vision and, in rare cases, heart-rhythm disturbances.5
Second-generation drugs bind selectively to H1 receptors and penetrate the brain far less, offering similar symptom relief with minimal sedation, said Trisha Ray, MD, clinical director of Allergy and Immunology at Beth Israel Deaconess Medical Center.
Risks that prompt calls for a “goodbye”
Authors of the February commentary cite multiple concerns:1
• Impaired driving—one study found diphenhydramine caused more lane deviation than a 0.10 percent blood-alcohol level, whereas fexofenadine had no effect.6
• Cognitive burden—cumulative use in adults 65 and older links to higher dementia risk.
• Pediatric reactions—children may become paradoxically agitated before slipping into deep sedation.
• Cardiac and anticholinergic effects—arrhythmias, dry eyes, constipation and urinary retention.
• Abuse potential—highlighted by the viral “Benadryl Challenge,” which led to hospitalizations and deaths.7
Because modern non-sedating agents control symptoms just as well, the authors conclude that diphenhydramine should be removed from pharmacy shelves.
Current clinical guidance agrees. U.S. allergy societies have recommended second-generation antihistamines for rhinitis since 2020, citing improved safety.9 Similar advice appears in international hives guidelines.10
Where Benadryl still fits
Specialists acknowledge niche roles. The drug’s rapid onset—15–30 minutes versus 20–60 for newer agents—makes it helpful in acute allergic flares and as a short-acting sedative before procedures, said Jessica Hui, MD, a pediatric allergist at National Jewish Health. It can also be useful when a brief duration of action is preferred.
Nonetheless, for routine hay-fever relief or chronic hives, experts recommend newer antihistamines, which last longer and can be dosed consistently without next-day grogginess.
“Most patients just want to breathe and function,” Ray said. “With second-generation options available, there’s little reason to reach for Benadryl first—except habit.”
- ▶ Hesperidin
- ▶ Citrus Bioflavonoids
- ▶ Plant Extract
- ▶ lycopene
- ▶ Diosmin
- ▶ Grape seed extract
- ▶ Sea buckthorn Juice Powder
- ▶ Fruit Juice Powder
- ▶ Hops Extract
- ▶ Artichoke Extract
- ▶ Mushroom extract
- ▶ Astaxanthin
- ▶ Green Tea Extract
- ▶ Curcumin
- ▶ Horse Chestnut Extract
- ▶ Other Product
- ▶ Boswellia Serrata Extract
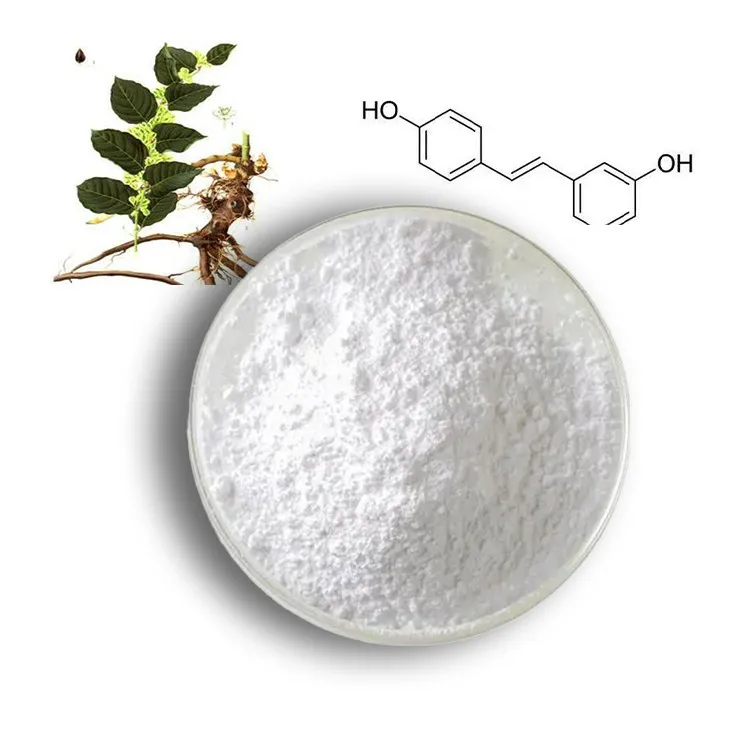
- ▶ Resveratrol
- ▶ Marigold Extract
- ▶ Grape Leaf Extract
- ▶ New Product
- ▶ Aminolevulinic acid
- ▶ Cranberry Extract
- ▶ Red Yeast Rice
- ▶ Red Wine Extract
-
Ivy Extract
2025-07-31
-
Licorice Root Extract Powder
2025-07-31
-
Konjac Powder
2025-07-31
-
Plantain extract
2025-07-31
-
Chia Seed Powder
2025-07-31
-
Resveratrol extract
2025-07-31
-
Centella Asiatica Extract
2025-07-31
-
Dandelion Root Extract
2025-07-31
-
Hawthorn Extract
2025-07-31
-
Lotus leaf extract
2025-07-31