- 0086-571-85302990
- sales@greenskybio.com
What is Aminolevulinic Acid Disease? An In-Depth Overview
2025-06-07

Aminolevulinic acid (ALA) is a naturally occurring compound vital to the body’s production of heme, the oxygen-binding component of hemoglobin. While the molecule itself is essential for the normal functioning of red blood cells and cellular respiration, certain disruptions in its metabolism can lead to the accumulation of Aminolevulinic acid in the body, resulting in what is often referred to as “Aminolevulinic acid disease.” More specifically, this accumulation occurs in a group of rare metabolic disorders known as acute hepatic porphyrias (AHPs), of which acute intermittent porphyria (AIP) is the most common. This article explores the scientific and clinical perspectives on aminolevulinic acid disease, its biochemical basis, clinical presentation, diagnosis, and treatment.
Understanding Aminolevulinic Acid and Heme Biosynthesis
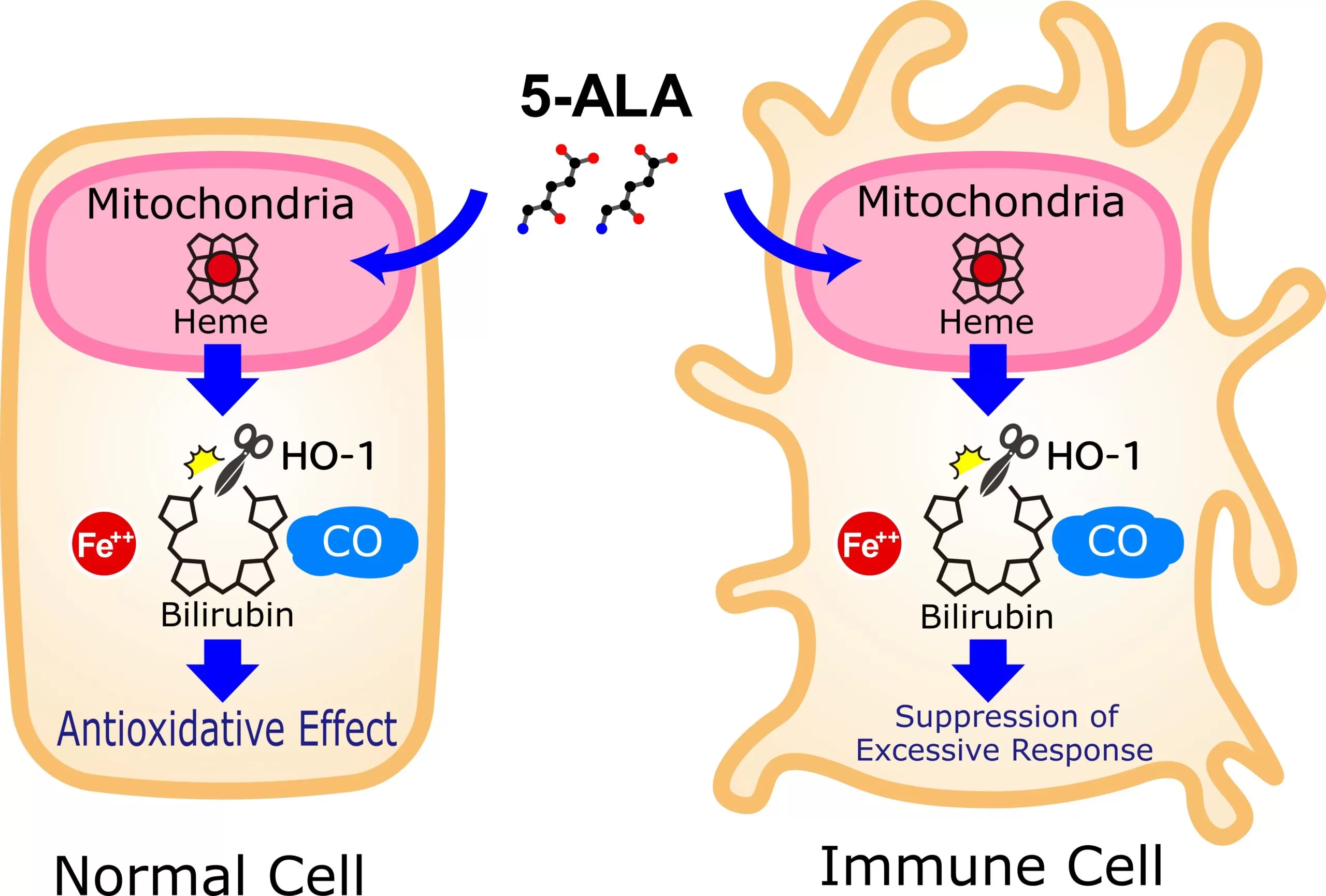
Aminolevulinic acid plays a foundational role in the heme biosynthesis pathway. Heme is a critical prosthetic group found in hemoglobin, myoglobin, and various enzymes involved in oxygen transport, detoxification, and energy production. ALA is synthesized in the mitochondria from glycine and succinyl-CoA in a reaction catalyzed by ALA synthase (ALAS), considered the rate-limiting step in heme biosynthesis.
Following its synthesis, ALA enters a multi-step pathway involving several enzymes and intermediates. Disruptions at various steps of this pathway, typically due to inherited enzyme deficiencies, result in the buildup of specific precursors, including ALA itself. The accumulation of ALA, along with porphobilinogen (PBG), is responsible for the hallmark features of acute porphyrias.
Aminolevulinic Acid Disease: Acute Hepatic Porphyrias
The phrase “aminolevulinic acid disease” is not a formal medical diagnosis but rather a descriptive term for disorders characterized by a pathological accumulation of ALA. This primarily refers to four forms of acute hepatic porphyrias: acute intermittent porphyria (AIP), variegate porphyria, hereditary coproporphyria, and ALA dehydratase deficiency porphyria (also called Dossphyria). Of these, ALA dehydratase deficiency porphyria (ALAD-P) is the most directly linked to ALA accumulation because the enzymatic defect prevents ALA’s conversion to the next molecule in the heme pathway.
Biochemical Mechan
In healthy individuals, ALA is efficiently converted to PBG, and then through a of steps, to heme. However when ALA dehydase (also known asBG synthase), the enzyme responsible for catalyzing this conversion, is deficient or dysfunctional (as in ALAD-P), ALA accumulates to toxic. Other forms of acute hepatic porphyria, especially AIP, are caused by deficiencies in enzymes further downstream in the pathway, allowing A and PBG to build up.
When the body’s demand for heme increases ( as during illness, hormonal fluctuations, or exposure to drugs), the production of ALA ramps up in an attempt to boost heme synthesis. If a metabolic bottleneck prevents further progression, ALA and P accumulate, triggering the symptoms of acute porphyria.
Clinical Presentation: Signs
The clinical features aminolevulinic acid disease are largely due to the toxic effects ofLA and related intermediates on the nervous. Classic symptoms of an “acute porric attack” include:
- Severe abdominal: the most common symptom, often accompanied by nausea, vomiting and constipation.
Neurological disturbances: including peripheral neuropathy (weakness, tingling or paralysis), changes (anxiety, hallucinations, confusion), and seizures in severe cases- Autonomic nervous system dysfunction: manifesting as rapid heart rate, hypertension, and sweating.
- Dark or reddish urine: due to the excretion ALA and PBG, which can darken upon standingAttacks are typically precipitated by certain medications, infections, fasting, stress, or hormonal changes (such as during the menstrual cycle). Without prompt treatment, acute attacks can progress life-threatening complications such as respiratory failure or cardiac arrhythmias.
Diagnosis
Diagnosis relies on a combination of clinical suspicion, family history, and laboratory analysis. Key diagnostic steps include:
- Urine testing: showing elevated levels ofLA and PBG during an acute attack.
- Genetic: to confirm mutations in the genes encoding heme bios enzymes.
- Additional laboratory studies: such as measurements of liver function,, and magnesium, and exclusion of other causes of neuropathy or abdominal pain.
The rarity and variable presentation of aminvulinic acid disease result in delayed or missed diagnoses, underscoring the importance of clinician awareness.
Treatment and Management
Treatment is focused on hal the accumulation of toxic intermediates, managing, and preventing attacks. Key approaches include:
- Intravenous hemin: Supplementing hemin “turns off” the endogenous production ofLA, thereby reducing the accumulation of ALA and PBG.
- Removal or avoidance of triggers: certain drugs (barbiturates, sul antibiotics), alcohol, extreme caloric restriction, and hormonal triggers- Supportive care: Hospitalization may be necessary during acute attacks pain control, anti-nausea medications, fluid, and monitoring of vital signs.
- New therapies: Recently, Givosiran, an RNA interference therapeutic, has been approved for certain hepatic porphyrias, reducing circulating ALA and decreasing the frequency of attacks.
Prognosis
With timely diagnosis and appropriate management, most individuals with aminolevulin acid disease can avoid severe complications and lead relatively normal. Frequent or severe attacks,, can result in long-term neurological deficits or organ dysfunction.
Conclusion
Aminolevulinic acid disease a shorthand term for a group of rare, inherited metabolic disorders known as acute porphyrias. The condition results from deficiencies in enzymes of heme biosynthetic pathway, leading to the accumulation of potentially toxic intermediates principally ALA. Prompt recognition, diagnosis, and management crucial to prevent life-threatening attacks and improve patient outcomes. Ongoing research into the molecular foundations and new treatments continues advance care and quality of life for affected individuals.
- ▶ Hesperidin
- ▶ citrus bioflavonoids
- ▶ plant extract
- ▶ lycopene
- ▶ Diosmin
- ▶ Grape seed extract
- ▶ Sea buckthorn Juice Powder
- ▶ Beetroot powder
- ▶ Hops Extract
- ▶ Artichoke Extract
- ▶ Reishi mushroom extract
- ▶ Astaxanthin
- ▶ Green Tea Extract
- ▶ Curcumin Extract
- ▶ Horse Chestnut Extract
- ▶ Other Problems
- ▶ Boswellia Serrata Extract
- ▶ Resveratrol Extract
- ▶ Marigold Extract
- ▶ Grape Leaf Extract
- ▶ Coix Seed Extract
- ▶ Aminolevulinic acid
- ▶ Cranberry Extract
-
The best lemon juice powder in nature.
2025-06-07
-
Organic Vitamin K2 Powder Suppliers
2025-06-07
-
Bulk purchase of L - tyrosine.
2025-06-07
-
Vitamin K2 Manufacturers
2025-06-07
-
Berberis aristata Extract
2025-06-07
-
Red Vine Extract
2025-06-07
-
Shikone Extract
2025-06-07
-
Alfalfa Meal
2025-06-07
-
Artichoke Extract
2025-06-07
-
Beetroot Powder
2025-06-07
-
Kupilu Extract
2025-06-07
-
Calendula Extract
2025-06-07
-
Okra Extract
2025-06-07
-
Thunder God Vine Extract
2025-06-07